Comments on the Corpus
Luteum and Some Related Aspects Adapted
excerpt from "Novas Perspectivas em Ginecologia" |
|
Let us talk
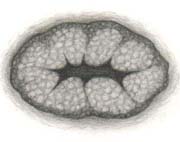
a little about the corpus luteum, the ovarian structure responsible for
the production of progesterone during the second phase of the menstrual
cycle ( and also the first two or three months of pregnancy ). After ovulation
( which is triggered by the pituitary ovulatory peak of LH ) and the subsequent
luteinization of the granulosa cells of the ruptured ovarian follicle,
there is a change in the enzymatic system of these cells and, instead
of producing mostly estrogens ( as they did ), they begin producing mainly
high levels of progesterone and only some estrogens. On the other hand,
the also luteinized theca cells begin producing mostly estrogens. Therefore,
the corpus luteum produces not only progesterone but also estrogens.
During the
ovarian cycle, the corpus luteum exhibits a considerably steady life period
of about 12 to 14 days. In this way, comparing the two phases of the ovulatory
cycles ( the follicular and the luteinic ), the luteinic phase is the
one that presents a more predictable duration. The corpus luteum seems
to possess some intrinsic capability of self-regulation. Even so, there
are indications that it depends on normal levels of LH and prolactin for
maintaining itself. The corpus luteum involution between its 10th and
14th days of existence seems to be due to a reduction in its LH-receptors,
what makes its responsivity to the LH become smaller. Some authors observe
that, on a short term basis, the LH action upon the corpus luteum causes
a reduction in the LH-receptors of the lutein cells, and that this may
be the main mechanism responsible for limiting the normal lutein function
to 12-14 days. It has also been postulated the possible existence of luteolithic
factors causing the involution of the corpus luteum after its 10th to
12th days of activity ( See Note below
).
There are also
curious aspects concerning the estrogens/progesterone relationships in
women. However, some previous considerations become necessary here. Initially,
from the exclusively biological point of view related to the original
reproductive purpose of the actions of the sexual hormones, it is
known that in each menstrual cycle estrogens and progesterone produce
a series of sequential transformations in the female genitals intended
to prepare it for fertilization, implantation and the beginning of the
egg's development. In the course of the first phase of the cycle, the
estrogens produce specific changes in the woman's sexual organs that are,
after ovulation and during the second phase, completed by other changes
induced by progesterone. If pregnancy occurs, the main function of progesterone
changes into the maintenance of this condition.
All of these
effects of the sexual steroids are well-known to present-day gynecology,
and it is not my purpose here to go into details about them. Also, I want
to make it clear that I do not intend here to discuss the interrelations
between estrogens and progesterone from the point of view of the reproductive
finality of the actions of these hormones. My opinion is that the
entire human constitution by far transcends, existentially, many of its
original biological purposes. It is a fact that almost all modern women
only desire to become pregnant in a few moments in their whole lives.
During most of their fertile years, pregnancy is undesired and avoided
and, if it happens accidentally, it is almost always interrupted by an
intentional abortion. Usually women only want to know that they are potentially
fertile, that is, capable of having children, but only when they desire
and if they so desire. Therefore I think it is much more relevant to talk
about the estrogens/progesterone relationships from the point of view
of women in their habitual state, which is the one of non-pregnant women.
An adequate balance between the
actions of estradiol, estrone and progesterone is of fundamental importance
in gynecologic physiology. This is so because, besides the progesteronic
actions that are complementary to those of the estrogens, progesterone also
exerts a "braking" action against the excessive proliferative
effect of the estrogens. The effects of hyperestrogenism mostly on the endometrium
and the breasts are well-known, causing hyperplastic changes in the endometrial
glands and in the mammary ducts, acini and connective tissue.
The endometrial hyperplastic changes
clinically manifest themselves through excessive or prolonged menstrual
bleedings ( menorrhagia and hypermenorrhea ), and the mammary ones by thickenings
of the breast parenchyma and the appearance of nodules in it ( traditionally
known as "functional mastopathies" ). The problem is that some
special types of such hyperplastic lesions can be pre-carcinogenic. In this
way, the production of progesterone at adequate levels during the second
phase of the cycle is fundamental for preventing the appearance and development
of these pathologies ( mostly in the endometrium, since presently some of
the anti-proliferative effects of progesterone on the breasts are being
questioned by several authors ).
In order to have good levels of
progesterone, the adequate formation of the corpus luteum - which usually
results from the ovulatory process - is quite necessary. Even so, there
are cases of luteinization of follicles that do not succeed in ovulating,
a phenomenon known as "LUF" ( luteinized unruptured follicles
). However, as we do not know how frequent this luteinization of unruptured
follicles may be, we must continue considering the occurrence of ovulation
as a basic condition for the corpus luteum formation in normal circumstances.
Nevertheless, for women having
an active sexual life, most of the time frequent ovulations are beneficial
on the one hand and problematic on the other. They are beneficial for allowing
the formation of the corpus luteum and the adequate progesterone production,
preventing the appearance of the already mentioned endometrial and mammary
alterations. They are problematic for creating the constant risk of pregnancy,
with all its implications, problems and worries. Thus, here we are faced
with one more of the several ambivalent and paradoxical situations typical
of female nature.
Fortunately,
with the hormonal contraceptives that contain a correct balance in their
doses of synthetic estrogens and progestins, it is possible to provide
women with efficient contraceptive guarantees and, at the same time, with
a relative balance between estrogenic and progestogenic effects. For details
on the "Pill," see my article "Oral
Hormonal Contraceptives".
Note:
Here we must remember that, when pregnancy occurs, the quick appearance
of the chorionic gonadotropic hormone ( CGH ) produced by the egg begins
stimulating the corpus luteum, impeding its regression and transforming
it into the corpus luteum of pregnancy. This structure remains in activity
during the first trimester of gestation.
![]()
Nelson Soucasaux is a
gynecologist dedicated to Clinical, Preventive and Psychosomatic Gynecology.
Graduated in 1974 by Faculdade de Medicina da Universidade Federal do
Rio de Janeiro, he is the author of several articles published in medical
journals and of the books "Novas Perspectivas
em Ginecologia" ("New Perspectives in Gynecology")
and "Os Órgãos Sexuais Femininos:
Forma, Função, Símbolo e Arquétipo" ("The
Female Sexual Organs: Shape, Function, Symbol and Archetype"),
published by Imago Editora, Rio de Janeiro, 1990, 1993.
![]()
![]()
[ Home
] [ Consultório (Medical Office)
] [ Obras Publicadas (Published Works)
]
[ Novas
Perspectivas em Ginecologia (New Perspectives in Gynecology)
]
[ Os
Órgãos Sexuais Femininos (The Female Sexual Organs)
]
[ Temas Polêmicos (Polemical Subjects)
] [ Tópicos Diversos (Other
Topics) (Part 1) ]
[ Tópicos Diversos (Other
Topics) (Part 2) ] [ Tópicos
Diversos (Other Topics) (Part 3) ]
[ Tópicos Diversos (Other
Topics) (Part 4) ] [ Ilustrações
(Illustrations) ]
![]()